Abstract
Background: Strokes are a common and serious complication of Sickle Cell Disease (SCD). It is the most common cause of stroke in the pediatric population. The risk of recurrent strokes continues into adulthood in SCD population. In this abstract, we quantify the burden of strokes in the SCD population and compare it against the background of strokes in the non-SCD population.
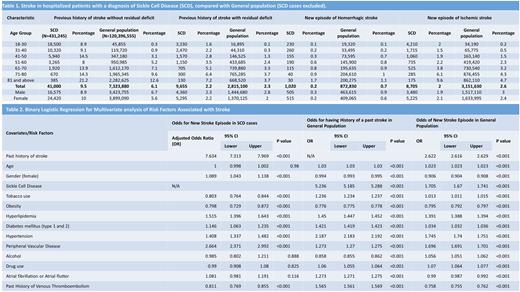
Methods: Adult cases with SCD were identified by the International Classification of Disease 10th Revision Diagnosis codes from the National Inpatient Sample Database for 2016-2019. The cases were distributed into age groups based on decades (18-30, 31-40, 41-50, 51-60, 61-70, 71-80; and 81 and above). Cases were identified for the presence of a history of a prior stroke [PMHS] with residual deficits, PMHS without deficits, a new episode of a hemorrhagic stroke, and a new episode of ischemic stroke. Binary logistic regression was performed for multivariate analysis to assess the effect of risk factors that are associated with stroke (age, gender, tobacco use, alcohol, hyperlipidemia [HLD], atrial fibrillation/atrial flutter, hypertension [HTN], peripheral vascular disease [PVD], obesity, diabetes mellitus [for both type 1 and 2], drug use, previous history of venous thromboembolism, and SCD). Please note that "non-SCD” represents only the cases excluding SCD patients. For regression analysis of the "general population", both SCD and non-SCD patients are included. The results are statistically weighted.
Results: 431,245 (0.36%) cases with SCD were identified from a total of 120,396,555 cases. The percentages are reported in ascending order of age by decade (18-30, 31-40, 41-50, 51-60, 61-70, 71-80; and 81 and above). The percentages of SCD cases with PMHS without deficits were 8.9, 9.1, 14.5, 8, 13.9, 14.3, and 21.2, respectively, while those for non-SCD cases were 0.3, 0.9, 3.1, 5.2, 7.1, 9.6, and 12.6 respectively. The percentages of SCD cases with PMHS with residual deficit were 1.6, 2.2, 2.8, 3.5, 5.1, 6.4, and 7.2, respectively, while those for non-SCD cases were 0.1, 0.3, 1.3, 2.4, 3.3, 3.7 and 3.7 respectively. The percentages of SCD cases with a new episode of an ischemic stroke were 2, 1.5, 1.9, 2.2, 3.8, 6.1, and 9.6, respectively, while those for non-SCD cases were 0.2, 0.5, 1.5, 2.3, 3.2, 4.3, and 4.7 respectively. The percentages of SCD cases with a new episode of hemorrhagic stroke were 0.1, 0.2, 0.3, 0.6, 0.8, 0.9, and 1.7, respectively, while those for non-SCD cases were 0.1, 0.2, 0.7, 0.8, 0.9, 1, and 1.1 respectively. The comparisons can be seen side by side in Table 1. Upon multivariate analysis of the general population to assess the effect of risk factors on PMHS, the remarkable odds ratios (OR) were: SCD with OR 5.24 (Confidence Interval 5.19-5.29, P<0.001) and HTN 2.19 (2.183-2.192, P<0.001). Multivariate analysis for a new episode of stroke in the general population showed that PMHS had an OR of 2.62 (2.61 - 2.63, P<0.001), HTN 1.745 (1.740-1.751, P<0.001), SCD 1.705 (1.67-1.74, P<0.001) and PVD 1.67 (1.65-1.70, P<0.001). On multivariate analysis for a new episode of stroke in SCD cases, notable results were PMHS with an OR of 7.47 (7.16-7.80, P<0.001), HTN 1.39 (1.32-1.46, P<0.001), HLD 1.58 (1.45-1.71, P<0.001), and tobacco use 1.25 (1.19-1.32, P<0.001). The OR for other risk factors can be reviewed in Table 2.
Conclusion: The number of strokes in SCD increases with age. The difference between SCD and non-SCD groups is most pronounced in the younger population. This gap narrows in the fifth decade when the incidence of strokes rises in the general population. PMHS is strongly correlated with new episodes of stroke. Aggressive management of SCD in the younger population, along with optimal risk factor modification (control of diabetes, HTN, HLD, smoking avoidance/cessation) is desirable to decrease the risk of stroke. Further research in this direction is warranted.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal